introduction
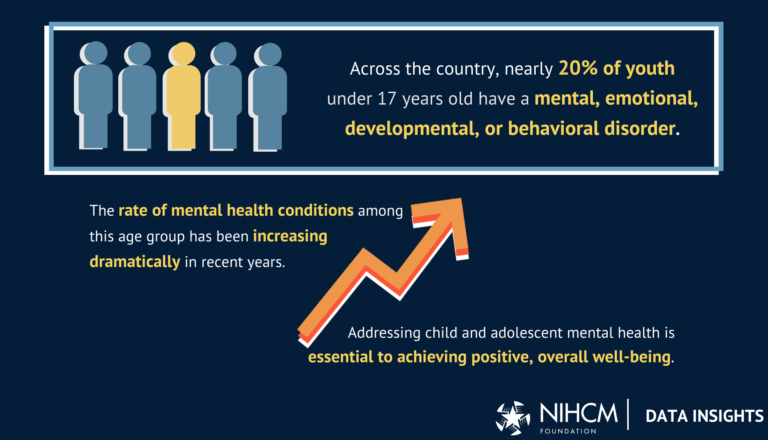
Approximately one in five children has a mental, emotional or behavioral disorder.
-
Source 1: Agency for Healthcare Research and Quality Assessment, 2022 National Healthcare Quality and Disparities Report, 2022
-
Source 2: Christina D. Bethell et al., Child and Adolescent Psychiatry Clinics of North America, Social and Relational Health Risks and Common Mental Health Problems in U.S. Children: The Role of Family Resilience and Connectedness in Promoting Social-Emotional and School-Related Outcomes, 2022
Mental health concerns are on the rise.
-
Source 1: Zara Abrams, American Psychological Association, 2023 Trends Report: Children’s Mental Health is in Crisis. Here’s what Psychologists are doing to help. 2023
-
Source 2: Jianmin Piao et al., European Child & Adolescent Psychiatry, Alarming changes in the global burden of mental disorders in children and adolescents between 1990 and 2019: a systematic analysis for the Global Burden of Disease Study, 2022
The Importance of Addressing Mental Health: U.S. Surgeon General, U.S. Public Health Service, Protecting Youth Mental Health: Recommendations from the U.S. Surgeon General, 2021
Rising rates of mental illness and suicide
Mental health issues are a leading cause of disability and poor health. U.S. Department of Health and Human Services, Office of the Surgeon General, Youth Mental Health, 2021
Several mental disorders often occur together.
-
Source 1: Centers for Disease Control and Prevention, Data and Statistics, 2023
-
Source 2: Reem M. Ghandour et al., Journal of Pediatrics, Prevalence and Treatment of Depression, Anxiety, and Behavioral Problems in U.S. Children, 2019
Age at Onset of Psychiatric Disorders: Ronald C. Kessler et al., JAMA Psychiatry, Lifetime Prevalence and Age-of-Onset Distribution of DSM-IV Disorders in a Replication of the National Comorbidity Survey, 2005
-
Additional resources: Martha Hostetter and Sarah Klein, Commonwealth Fund, “Transforming Care: Closing the Gaps in Access to Mental Health Treatment for Teens and Young Adults,” 2022
diagnosis & Suicide rate
Anxiety, depression, mood disorders, and behavioral disorders are the most common mental illnesses. American College of Obstetricians and Gynecologists, Adolescent Mental Disorders, 2017
Diagnosis through 2020: Lydie A. Lebrun-Harris et al., JAMA Pediatrics, Five-Year Trends in U.S. Children’s Health and Well-Being, 2016-2020, 2022
Severe depressive episodes are on the rise.
-
2011 – 2020: Substance Abuse and Mental Health Services Administration, 2020 National Survey on Drug Use and Health, Chapter 9: Youth Mental Health Tables, Table 11.2 B – Past-Year Major Depressive Episodes: Persons Ages 12-17, by Demographic Characteristics, Percentages, 2004 – 2020, 2020
- 2021: Substance Abuse and Mental Health Services Administration, 2021 National Survey on Drug Use and Health, Chapter 7: Youth Mental Health Tables, Table 7.7B – Major Depressive Episode (MDE) or MDE with Severe Impairment in the Past Year: Persons Aged 12-17, Past-Year Depression Treatment Visits: Persons Aged 12-17 with MDE and Persons Aged 12-17 with MDE with Severe Impairment in the Past Year, by Demographic Characteristics, Percentage, 2021
Suicide rates among youth and adolescents are also rising: National Center for Health Statistics, Centers for Disease Control and Prevention, “Suicide and Homicide Mortality Rates Among Youth and Young Adults Ages 10-24: United States, 2001-2021, 2023.”
Suicide is the second leading cause of death: CDC Wonder, Centers for Disease Control and Prevention, Underlying Causes of Death, 2018 – 2021, Single Race, 2023
Mental health and suicide rates vary
Mental Health Rates Vary by Race and Ethnicity: Jennifer A. Hoffman et al., Pediatrics, American Academy of Pediatrics, Disparities in Children’s Mental and Behavioral Health, 2022
American Indians and Alaska Natives had the highest suicide rates: Nirmita Panchal, Kaiser Family Foundation, Recent Trends in Youth Mental Health and Substance Use, 2024
Rural Mental Health:
-
Rural youth experience higher rates of mental illness: Kelly J. Kelleher and William Gardner, New England Journal of Medicine, “Out of Sight, Out of Mind – Behavioral and Developmental Care for Rural Children,” 2017
-
Suicide rates are high among youth attending rural health facilities: Jennifer A. Hoffman et al., Pediatrics, American Academy of Pediatrics, Pediatric Mental and Behavioral Health Disparities, 2022
-
Rural Youth Have Less Access to Mental Health Services: National Institutes of Health, NIH Research Matters, Rural Youth Often Lack Access to Suicide Prevention Services, 2020
-
Rural youth have to travel farther to access mental health services: Blake Berryhill et al. “Rural Mental Health, Treating Adolescent Depression and Anxiety in Rural Schools: A Systematic Review,” 2022
Women are more likely to attempt suicide, but men are more likely to die by suicide.
-
Source 1: Nirmita Panchal, Kaiser Family Foundation, Emerging Trends in Youth Mental Health and Substance Use, 2024
-
Source 2: WISQARS Fatal and Nonfatal Data Exploration, Centers for Disease Control and Prevention, Exploration of Fatal Injury Data Visualization, 2024
LGBTQ+ Mental Health:
Teens with disabilities are more likely to have mental, emotional, or behavioral health disorders.
-
Source 1: Shalini Lal et al., Frontiers in Rehabilitation Sciences, Mental Health Issues in Adolescents and Young Adults with Childhood-Onset Physical Disabilities: A Scoping Review, 2022
-
Source 2: Jackie Carey, Applied Health Sciences, Helping Teens with Disabilities Prevent and Treat Depression and Anxiety, 2021
Biology and social determinants shape youth mental health
Some Factors Shape Youth Mental Health: U.S. Public Health Service, U.S. Public Health Service, Protecting Youth Mental Health: Recommendations from the U.S. Surgeon General, 2021
Life experiences: How COVID-19 impacts mental health
COVID-19 has worsened children’s mental health:
-
Source 1: Sherry Everett Jones et al., Morbidity and Mortality Weekly Report, Centers for Disease Control and Prevention, Mental Health, Suicidality, and Connectedness Among High School Students During the COVID-19 Pandemic—Youth Behaviors and Experiences Survey, United States, January-June 2021, 2022
-
Source 2: Zara Abrams, American Psychological Association, 2023 Trends Report: Children’s Mental Health is in Crisis. Here’s What Psychologists are Doing to Help. 2023
-
Source 3: Nicole Racine et al., JAMA Pediatrics, Global Prevalence of Depression and Anxiety Symptoms in Children and Adolescents During the COVID-19 Outbreak, 2021
The pandemic has exacerbated existing mental health challenges, especially for vulnerable populations: U.S. Department of Health and Human Services, Office of the Surgeon General, Youth Mental Health, 2021
Emergency Department Visits on the Rise: Rebecca T. Reeve et al., Morbidity and Mortality Weekly Report, Centers for Disease Control and Prevention, Mental Health-Related Emergency Department Visits Among Children Under 18 Years of Age During the COVID-19 Pandemic – United States, January 1-October 17, 2020, 2020d
Inadequate treatment of mental illness
Mental illnesses are often underdiagnosed and undertreated. Margarita Alegría, Melissa Vallas, and Andrés Pumariega, “Racial and Ethnic Disparities in Pediatric Mental Health in Child and Adolescent Psychiatry Clinics in North America,” 2010
More than 50% of youth under the age of 18 did not receive mental health treatment in the past year: Daniel G. Whitney and Mark D. Peterson, JAMA Pediatrics, US National and State-Level Prevalence of Mental Health Disorders and Disparities in Children’s Mental Health Care Utilization, 2019
Unmet need is greater among racial and ethnic minorities. Tracey L. Henry et al., Journal of Primary Care & Community Health, “A Closer Look at Mental Health Treatment Differences: Effectiveness of Mental Health Treatment by Provider Type Among Racial and Ethnic Minorities,” 2020
State-level differences
The percentage of children and adolescents not receiving mental health treatment varies by state. Daniel G. Whitney and Mark D. Peterson, JAMA Pediatrics, US National and State-Level Prevalence of Mental Health Disorders and Disparities in Children’s Mental Health Care Utilization, 2019
Reasons for treatment interruption
When mental health issues go undiagnosed, untreated, or not properly treated, they can interfere with your daily life.
-
Source 1: Centers for Disease Control and Prevention, Children’s Mental Health, What is Children’s Mental Health?, 2023
-
Source 2: Mental Health America, Awareness of Children’s Mental Health Issues, 2024
Cost of Care: National Mental Health Council, Study Finds Lack of Access is Root Cause of America’s Mental Health Crisis, 2018
Shortage of Mental Health Professionals: Hemangi Modi, Kendall Orgera, Atul Grover, Association of American Medical Colleges Institute, Examining Barriers to Mental Health Care in the United States, 2022
Awareness of social prejudice
-
Source 1: Nirmita Panchal, Kaiser Family Foundation, Emerging Trends in Youth Mental Health and Substance Use, 2024
-
Source 2: Amelia Gulliver, Kathleen M. Griffiths, Helen Christensen, BMC Psychiatry, “Barriers and facilitators to mental health help-seeking among young people: a systematic review,” 2010
Long Waiting Times: Stella McLaughlin et al., BMJ Open, Interventions to reduce waiting times for young people seeking mental health services: A scoping review protocol, 2023
Lack of knowledge
-
Source 1: Nirmita Panchal, Kaiser Family Foundation, Emerging Trends in Youth Mental Health and Substance Use, 2024
-
Source 2: National Council on Mental Health, Study Finds Lack of Access is Root Cause of America’s Mental Health Crisis, 2018
The Lack of Culturally Competent Care: Alana N. Rice and Suzanne C. Harris, Journal of the American Pharmacists Association, The Challenge of Cultural Competency in Mental Health Care, 2021
Strategies to address children’s mental health
Creating a framework to promote mental health
Addressing Youth Mental Health Disparities: National Institute of Mental Health, Strategic Framework for Addressing Youth Mental Health Disparities: FY2022-FY2031, 2022
Raising mental health awareness:
-
Source 1: Centers for Disease Control and Prevention, Promoting Social, Emotional and Behavioral Learning, 2023
-
Source 2: Consortium for Academic, Social and Emotional Learning, SEL and Mental Health, 2023
Identifying Mental Health Needs Early: U.S. Department of Health and Human Services, Public Health Service, Youth Mental Health, 2024
Investing in stakeholder engagement
Incorporate strategies to prevent suicide:
-
Source 1: Centers for Disease Control and Prevention, Prevention Strategies, 2022
-
Source 2: Eric J. Siegel and Mara H. Rahmandar, “Healthy Kids,” American Academy of Pediatrics, “Suicide Prevention: 12 Things Parents Can Do,” 2023
Improving mental health support
Expand workforce capabilities:
Implementing Evidence-Based Programs: U.S. Department of Health and Human Services, Public Health Service, Youth Mental Health, 2024
Providing ongoing support:
-
Source 1: U.S. Department of Health and Human Services, Office of the Surgeon General, Youth Mental Health, 2024
-
Source 2: Resources for Integrated Care, Resources for Plans and Providers for Medicare-Medicaid Integration, Appropriate Care for People with Disabilities, 2024
Utilizing non-traditional settings of care
-
Source 1: Vicki Waccino, Brookings Institution, Moving Mental Health Care Out of the Office, 2023
-
Source 2: Sydney D’Aniello et al., Mental Health Alliance, “Responding to the Youth Mental Health Crisis: Urgent Need for More Education, Services and Support,” 2021
-
Source 3: Centers for Disease Control and Prevention, Children’s Mental Health Services Policy Brief, 2023
Explore complementary approaches to mental health
-
Source 1: Brad Bowins, MD, National Alliance on Mental Illness, 7 Actions to Improve Your Mental Health
-
Source 2: National Alliance on Mental Illness, Complementary Health Approaches, 2023
-
Source 3: Aksha M Memon et al., Indian Journal of Psychiatry, “Role of Online Social Networking on Intentional Self-Harm and Suicidality among Adolescents: A Systematic Review of the Literature,” 2018
-
Source 4: Matteo Briguglio et al., Neuropsychiatric Disorders and Their Treatment, Healthy Diet, Physical Activity, and Sleep Hygiene (HEPAS) is a Winning Triad for Maintaining the Physical and Mental Health of Patients at Risk for and with Neuropsychiatric Disorders: Considerations for Clinical Practice, 2020