Study design and participants
A mixed-methods prospective multicenter epidemiological study using secondary data was performed. The study was conducted in four specialized geriatric hospitals in Rhineland-Palatinate, Germany. Inclusion criteria were completion of acute geriatric complex care in one of the participating clinics, age >70 years, geriatric multimorbidity, and life expectancy >12 months (Figure 2). Patients in the intervention group were recruited in one of the participating hospitals and received the new form of care. The control group was provided by data from the BARMER health insurance, the statutory health insurance provider in Germany (Scientific Data Warehouse (W-DWH)). Written informed consent was obtained from all patients to participate in the study. In the case of patients unable to consent, informed consent was obtained from their legal guardian.
A new form of care
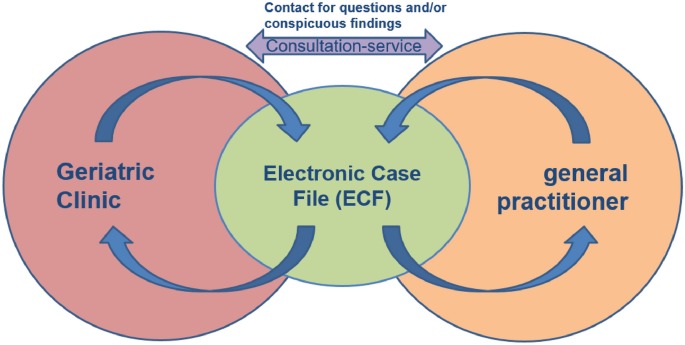
The new form of care revolves around a web-based Electronic Case File (ECF), which acts as a communication platform between the geriatric clinic and the participating general practitioners (GPs). In addition, a consultation service has been introduced to answer questions from the treating GPs and clinics and to monitor the medical appropriateness of the case file (see Figure 1).
Two-way interaction within the framework of new forms of care.
After fulfilling the inclusion criteria and giving written consent to participate in the study, the supervising research centre/discharge clinic entered the test results, assessments, progress reports, medication schedules and doctor’s letters into the ECF (Figure 2). The ECF did not require any additional or specialised software and was easily accessible from the project’s home page. The corresponding access data was sent by the research centre to the GP. The ECF was easily accessible by general practitioners (GPs) for further treatment. Thus, before the patient was discharged from the hospital and presented to the GP for the first time, the information could be seen via the ECF. It is the GP’s responsibility to maintain the ECF for one year, including quarterly updates on the patient’s condition and a basic geriatric assessment. Any changes in the patient’s condition, measures initiated and especially changes in medication should also be documented. The hospital geriatrician reviewed and inspected the current medication list together with a pharmacist specialising in geriatrics. In case of further enquiries or necessary actions, the medical consultation service contacted the GP either directly via the messenger function of the ECF or by phone using a specially set up number.

Description of the evaluation design.
Findings and statistical analysis
The primary outcome was the readmission rate within one year after discharge from inpatient geriatric care. The project consisted of five survey time points: a baseline survey during inpatient treatment in one of the participating geriatric clinics, followed by four regular outpatient consultations with a GP (HA1, HA2, HA3, HA4). Voluntary consultations with a GP were also available during the follow-up period, if required (Figure 2). Readmission rates for the control group were taken from BARMER W-DWH. Patients in the control group were matched 1:1 with patients in neo-formal geriatric care. For this purpose, age (± 2 years), sex (exact), and underlying diseases (ICD-10, 2 digits) were identified and matched in BARMER (W-DWH). To address possible differences in severity/intensity of treatment, patients were also matched with relative weights (and case severity, coefficient ± 0.5). Relative weights are multipliers (point values) of the base rate. Thus, it indicates the factor by which the base case value increases in the DRG system. A relative weight above 1 indicates a more complex case than the average case, and therefore a higher “case severity”. According to unpublished data from a health insurance company, about 70% of geriatric patients are readmitted at least once in a year after being admitted to the previous standard form of care. The average readmission rate for that year was 1.85 (5411 cases / year * 2931 insured persons). If we assume that the new form of care can reduce this rate to 1.30, then to hedge the difference between the two rates against chance with 0.05 alpha and 0.90 power, we would need to include 110 patients per care option. Thus, a total of 220 patients should be included in the study and followed to the end. It is important to keep in mind that readmissions are recurrent events and are likely to be correlated within patients. Furthermore, the number of cases should be increased to n = 275 due to the possibility of cluster effects within hospitals. Due to the advanced age of the patients, a relatively high dropout rate of up to 50% was expected, which means that 550 patients would need to be included.
To analyze the impact of the Covid-19 pandemic on hospitalization, we performed a multivariate Poisson regression analysis in the GerNe patient population. GerNe patients were divided into three groups: group 1 consisted of patients with a complete observation period before the first lockdown (March 22, 2020), group 2 consisted of patients with an observation period before and after March 22, 2020, and group 3 consisted of patients with all observation periods after March 22, 2020. As patients in group 2 were not clearly assigned, only patients in groups 1 and 3 were included in the regression analysis. Relevant confounding factors such as age, sex, relative weight, and level of care were also adjusted for.
Additionally, the GerNe project assessed several secondary outcomes, including level of care, living at home, vital status (death), medication (quality/quantity/change), quality of life (SF-8 questionnaire), functional status (Barthel index), and health care utilization costs.
Levels of care refer to the classification of individuals who require care due to health impairments or disabilities into different levels based on the degree of their needs. In the German care system, there are five levels of care (1–5), with care level 1 requiring the lowest level and care level 5 the highest level of support. The higher the care level, the more comprehensive the care services available. Changes in the level of care for GerNe patients were described objectively.2 Tests were used to compare GerNe patients and control individuals.
To measure quality of life, the Short-Form Health Survey 8 (SF-8) was used. It consists of eight items, which are translated into eight domains: physical functioning (PF), role physical functioning (RP), bodily pain (BP), general health perception (GH), vitality (VT), social functioning (SF), role emotional functioning (RE) and mental health (MH). All domains are reported with values between 0 and 100, with higher scores indicating better health. Patients self-filled the SF-8 at the start of the project and at their last GP visit (HA4). To assess quality of life, changes in the individual domains and scales were examined and compared with the German age- and sex-adjusted normative population.14Mean comparisons, effect sizes, and cross-tabulations were used to analyze changes over the course of the project.
The Barthel Index (BI) assesses a person’s ability to perform 10 basic activities of daily living, including eating, bathing, grooming, dressing, bowel and bladder control, toileting, transferring (e.g. from bed to chair), ambulation, and climbing stairs. Each activity is scored on a scale of 0 to 10, with higher scores indicating greater independence and functional ability. A maximum of 100 points can be earned.15Changes over the project period were analyzed using mean comparisons, effect sizes, and paired t-tests.
The use of new forms of care was assessed through the use of consultation services. The evaluation of the consultation service was descriptive. For this purpose, the number of contacts (use of the messaging function) and conversations (interactions with patients with multiple contacts) were given in absolute values.
Utilization of health services was recorded in case files, and this data was identified and analyzed in the BARMER control group of W-DWH.
The costs of hospital treatment (hospitalization) were calculated from the “base case rate,” a financial indicator in the health system that represents the monetary value of a standardized treatment case or a standardized unit of service.
ethics
The study was conducted in accordance with the principles of the Declaration of Helsinki and was voted in favor by the Ethics Committee of the Medical Association of Rhineland-Palatinate (Germany) on June 18, 2018 (No. 2018–13,347).
Consent to participate
Informed consent was obtained from all participants enrolled in the study.