Borders, T. F., Rohrer, J. E., Hilsenrath, P. E. & Ward, M. M. Why rural residents migrate for family physician care. J. Rural Health 16(4), 337–348. https://doi.org/10.1111/j.1748-0361.2000.tb00484.x (2000).
Google Scholar
Velasco Garrido, M., Zentner, A. & Busse, R. The effects of gatekeeping: a systematic review of the literature. Scand. J. Prim. Health Care 29(1), 28–38. https://doi.org/10.3109/02813432.2010.537015 (2011).
Google Scholar
Moore, A., Frank, C. & Chambers, L. W. Role of the family physician in dementia care. Can Fam Physician. 64(10), 717–719 (2018).
Google Scholar
Guan, X., Lan, T., Liao, W., Wu, X. & Pan, J. Exploring the effect of the primary care health workers number on infectious diarrhea morbidity and where the health resources should go. Sci. Rep. 12(1), 6060. https://doi.org/10.1038/s41598-022-10060-y (2022).
Google Scholar
Bindman, A. B. & Majeed, A. Primary care in the United States: Organisation of primary care in the United States. BMJ 326(7390), 631–634. https://doi.org/10.1136/bmj.326.7390.631 (2003).
Google Scholar
Kozhimannil, K. B. & Westby, A. What family physicians can do to reduce maternal mortality. Am. Fam. Physician. 100(8), 460–546 (2019).
Google Scholar
Phillips, R. L. Jr. et al. A Family Medicine Health Technology Strategy for Achieving the Triple Aim for US Health Care. Fam Med 47(8), 628–635 (2015).
Google Scholar
Carter, R., Lévesque, J. F., Harper, S. & Quesnel-Vallée, A. Measuring the effect of Family Medicine Group enrolment on avoidable visits to emergency departments by patients with diabetes in Quebec Canada. J. Eval Clin. Pract. 23(2), 369–376. https://doi.org/10.1111/jep.12627 (2017).
Google Scholar
Sohrabi, M. R., & Albalushi, R. M. Clients’ satisfaction with primary health care in Tehran: A cross-sectional study on Iranian Health Centers. J Res Med Sci. 16(6), 756–762. (2011).
Lankarani, K. B., Alavian, S. M. & Haghdoost, A. A. Family physicians in Iran: Success despite challenges. Lancet 376(9752), 1540–1541. https://doi.org/10.1016/S0140-6736(10)62029-6 (2010).
Google Scholar
Treharne, G. J., Carroll, R., Tan, K. K. H. & Veale, J. F. Supportive interactions with primary care doctors are associated with better mental health among transgender people: Results of a nationwide survey in Aotearoa/New Zealand. Fam. Pract. 39(5), 834–842. https://doi.org/10.1093/fampra/cmac005 (2022).
Google Scholar
Shang, X. et al. Residents’ awareness of family doctor contract services, status of contract with a family doctor, and contract service needs in Zhejiang Province, China: A cross-sectional study. Int. J. Environ. Res. Public Health 16(18), 3312. https://doi.org/10.3390/ijerph16183312 (2019).
Google Scholar
Statistical bulletin on the development of health care in China in 2021 https://www.gov.cn/xinwen/2022-07/12/content_5700670.htm, (2021).
National Health and Family Planning Commission: Transcript of the press conference of the National Health Council on 23 July 2021. http://www.nhc.gov.cn/xcs/s3574/202107/ea10acafc7d1493d820f6789c51cf571.shtml, 16 May 2024. (2021).
Wang, C. et al. Residents’ willingness to maintain contracts with family doctors: A cross-sectional study in China. J Gen. Intern. Med. 36(3), 622–631. https://doi.org/10.1007/s11606-020-06306-y (2021).
Google Scholar
Qing-Yan, S. I. Challenges and solutions for training about contractual Services for on-site Primary Physicians before transferring to the position of family doctors. Chin. Gen. Pract. 7, 22 (2018).
Wang, L. & Liu, W. Effects of Family Doctor Contract Services on the Health-Related Quality of Life Among Individuals with Diabetes in China: Evidence From the CHARLS. Front Public Health https://doi.org/10.3389/fpubh.2022.865653 (2022).
Google Scholar
Li, Z. et al. Family doctor contract services and health-related quality of life among patients with chronic diseases in rural China: What is the role of socioeconomic status?. Int. J. Equity Health 20(1), 191. https://doi.org/10.1186/s12939-021-01530-2 (2021).
Google Scholar
Xu, C. et al. The Impact of a Family Doctor Contract Service on Outcomes for Type 2 Diabetes Patients in Zhejiang Province. Asia Pac. J. Public Health 34(6–7), 643–648. https://doi.org/10.1177/10105395221113778 (2022).
Google Scholar
Lai, S. et al. The effects of family physician-contracted service on health-related quality of life and equity in health in China. Int. J. Equity Health 20(1), 15. https://doi.org/10.1186/s12939-020-01348-4 (2021).
Google Scholar
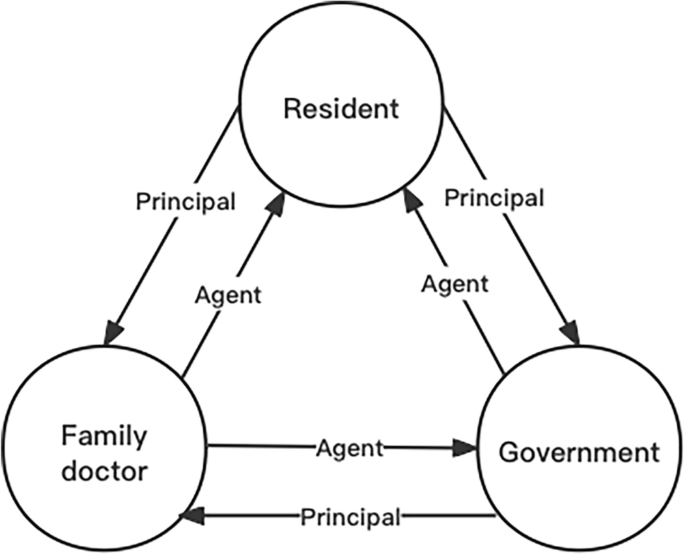
Vera-Hernández, M. Structural estimation of a principal-agent model: Moral hazard in medical insurance. Rand. J. Econ. 34(4), 670–693 (2003).
Google Scholar
Li, D., Su, M., Guo, X., Zhang, W. & Zhang, T. The effect of medical choice on health costs of middle-aged and elderly patients with chronic disease: Based on principal-agent theory. Int. J. Environ. Res. Public Health 19(13), 7570. https://doi.org/10.3390/ijerph19137570 (2022).
Google Scholar
Langer, A., Schröder-Bäck, P., Brink, A. & Eurich, J. The agency problem and medical acting: an example of applying economic theory to medical ethics. Med. Health Care Philos. 12(1), 99–108. https://doi.org/10.1007/s11019-008-9138-y (2009).
Google Scholar
Li, L., He, X. & Zhang, C. The impact of public policy of family doctor contracting on medical expenses from the perspective of residents at community level in China. Front. Psychol. https://doi.org/10.3389/fpsyg.2022.972904 (2023).
Google Scholar
Buchanan, A. Principal/agent theory and decision making in health care. Bioethics 2(4), 317–333 (1988).
Google Scholar
Hao, X., Yang, Y., Gao, X. & Dai, T. Evaluating the Effectiveness of the Health Management Program for the Elderly on Health-Related Quality of Life among Elderly People in China: Findings from the China Health and Retirement Longitudinal Study. Int. J. Environ. Res. Public Health 16(1), 113. https://doi.org/10.3390/ijerph16010113 (2019).
Google Scholar
Zhao, L., Zhang, K., Gao, Y., Jia, Z. & Han, S. The relationship between gender, marital status and depression among Chinese middle-aged and older people: Mediation by subjective well-being and moderation by degree of digitization. Front. Psychol. https://doi.org/10.3389/fpsyg.2022.923597 (2022).
Google Scholar
Olazarán, J. et al. Mild cognitive impairment and dementia in primary care: the value of medical history. Fam Pract. 28(4), 385–392. https://doi.org/10.1093/fampra/cmr005 (2011).
Google Scholar
Ware, J., Snoww, K., Kosinski, M. A., & Gandek, B. G. SF-36. Health survey: manual and interpretation guide. Health Assess. Lab (1993).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. Mini-mental state A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12(3), 189–198. https://doi.org/10.1016/0022-3956(75)90026-6 (1975).
Google Scholar
Snyder, et al. Cocreative customer practices: effects of health care customer value cocreation practices on well-being. J. Bus. Res. https://doi.org/10.1016/j.jbusres.2016.07.006 (2017).
Google Scholar
Baron, R. M. & Kenny, D. A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 51(6), 1173–1182. https://doi.org/10.1037/0022-3514.51.6.1173 (1986).
Google Scholar
Arwert, H. J., Groeneveld, I. F., Vliet Vlieland, T. P. M. & Meesters, J. J. L. Health Care Use and Its Associated Factors 5–8 Years after Stroke. J. Stroke Cerebrovasc. Dis. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104333 (2019).
Google Scholar
Yokokawa, D. et al. Relationship between the presence of primary care physicians and health-related quality of life. J. Gen. Fam. Med. 23(2), 87–93. https://doi.org/10.1002/jgf2.490 (2021).
Google Scholar
Zhou, Z. et al. Evaluating the effect of hierarchical medical system on health seeking behavior: A difference-in-differences analysis in China. Soc. Sci. Med. https://doi.org/10.1016/j.socscimed.2020.113372 (2021).
Google Scholar
Xu, X., Zhou, L., Ampon-Wireko, S. & Quansah, P. E. Assessing the mediating role of motivation in the relationship between perceived management support and perceived job satisfaction among family doctors in Jiangsu province China. Hum. Resour. Health 21(1), 71. https://doi.org/10.1186/s12960-023-00849-x (2023).
Google Scholar
Li, X. et al. The primary health-care system in China. Lancet 390(10112), 2584–2594. https://doi.org/10.1016/S0140-6736(17)33109-4 (2017).
Google Scholar
Wang, A. et al. How surface acting affects turnover intention among family doctors in rural China: The mediating role of emotional exhaustion and the moderating role of occupational commitment. Hum. Resour. Health 21(1), 3. https://doi.org/10.1186/s12960-023-00791-y (2023).
Google Scholar
Ye, J. et al. Burnout among obstetricians and paediatricians: A cross-sectional study from China. BMJ Open https://doi.org/10.1136/bmjopen-2018-024205 (2019).
Google Scholar
Arrow, K. J. Uncertainty and the welfare economics of medical care. Bull. World Health Organ. 82(2), 141–149 (2004).
Google Scholar
Sarvimäki, A. & Stenbock-Hult, B. Quality of life in old age described as a sense of well-being, meaning and value. J. Adv. Nurs. 32, 1025–1033. https://doi.org/10.1046/j.1365-2648.2000.01568.x (2000).
Google Scholar
Yang, S. et al. Do older people with cardiovascular-metabolic multimorbidity prefer to sign contracts for family doctor services? Evidence from a cross-sectional study in rural Shandong China. BMC Geriatr. 21(1), 579. https://doi.org/10.1186/s12877-021-02543-w (2021).
Google Scholar
Huang, S., Yin, A., Liu, Q. & Sun, X. Can the implementation of family doctor contracted service enable the elderly to utilize primary health care services more equally? empirical evidence from Shandong China. BMC Prim Care. 23(1), 31. https://doi.org/10.1186/s12875-022-01630-0 (2022).
Google Scholar
Sabbah, I., Drouby, N., Sabbah, S., Retel-Rude, N. & Mercier, M. Quality of life in rural and urban populations in Lebanon using SF-36 health survey. Health Qual. Life Outcomes. 1, 30. https://doi.org/10.1186/1477-7525-1-30 (2003).
Google Scholar
Sutarsa, I. N., Kasim, R., Slimings, C., Bain-Donohue, S. & Barnard, A. Effects of employing primary care doctors in hospital to improve the quality of care and health outcomes of rural patients: A systematic scoping review. Aust. J. Rural Health. 29(4), 492–501. https://doi.org/10.1111/ajr.12779 (2021).
Google Scholar
Wang, M. et al. Knowledge, attitudes and skills of dementia care in general practice: A cross-sectional study in primary health settings in Beijing China. BMC Fam. Pract. 21(1), 89. https://doi.org/10.1186/s12875-020-01164-3 (2020).
Google Scholar
Wang, M. et al. The needs of informal caregivers and barriers of primary care workers toward dementia management in primary care: A qualitative study in Beijing. BMC Fam. Pract. 19(1), 201. https://doi.org/10.1186/s12875-018-0890-7 (2018).
Google Scholar
Man, F. Y., Chen, C. X., Lau, Y. Y. & Chan, K. Therapeutic inertia in the management of hyperlipidaemia in type 2 diabetic patients: A cross-sectional study in the primary care setting. Hong Kong Med. J. 22(4), 356–364. https://doi.org/10.12809/hkmj154667 (2016).
Google Scholar
Chen, C., Xu, R. H., Wong, E. L. & Wang, D. The association between healthcare needs, socioeconomic status, and life satisfaction from a Chinese rural population cohort, 2012–2018. Sci. Rep. 12(1), 14129. https://doi.org/10.1038/s41598-022-18596-9 (2022).
Google Scholar
Sawicki, O. A. et al. Strong and sustainable primary healthcare is associated with a lower risk of hospitalization in high risk patients. Sci. Rep. 11(1), 4349. https://doi.org/10.1038/s41598-021-83962-y (2021).
Google Scholar
Kuiper, J. S. et al. Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res. Rev. 22, 39–57. https://doi.org/10.1016/j.arr.2015.04.006 (2015).
Google Scholar
Evans, I. E. M., Martyr, A., Collins, R., Brayne, C. & Clare, L. Social isolation and cognitive function in later life: A systematic review and meta-analysis. J. Alzheimers Dis. 70(s1), S119–S144. https://doi.org/10.3233/JAD-180501 (2019).
Google Scholar