The Democratic Republic of Congo (DRC) is experiencing the largest outbreak of the viral disease mpox on record, with tens of thousands of people infected as of June. In December 2022, the government declared it an epidemic.
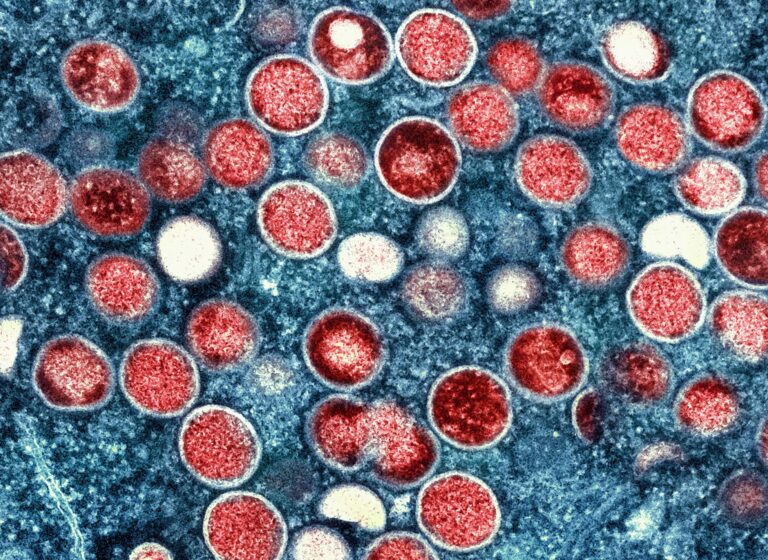
Formerly called monkeypox, MPOX disease is caused by the monkeypox virus and is usually zoonotic, meaning it can be transmitted from animals to humans.
The virus is endemic in densely forested areas of central and western Africa and is related to the virus that causes smallpox, which has now been eradicated. Smallpox can be fatal in severe cases, with the main symptoms being an itchy rash all over the body and fever. Vaccines can limit infection.
Although outbreaks are common in the DRC, health experts said a new strain has been discovered this time in part of the country.
Here’s what we know about the outbreak:
When did the mpox epidemic start?
The outbreak began in May 2022 in the eastern province of Kwango. It has since spread to 22 of the DRC’s 26 provinces, including the capital, Kinshasa.
Transmission, however, remains concentrated in the east of the country, with a high spread recorded in Kamituga, a mining town in the eastern province of South Kivu. Doctors have discovered a new strain of the virus in the town.
Since 2022, more than 21,000 cases have been reported and more than 1,000 deaths have been recorded, according to the World Health Organization (WHO). In 2023, a total of 14,626 cases and 654 deaths have been recorded.
This year alone, 7,851 cases have been recorded as of the end of May, including 384 deaths. Many of those infected are children under five (39%). Nearly two-thirds (62%) of those who have died from the disease are also children.
The provinces of Equateur, Sud-Ubangi, Sankuru and Sud-Kivu are among those most affected.
How many variants of mpox are there and are they deadly?
There have always been two types of mpox, also called clades.
Clade 2 is less deadly. This is the type of virus that spread in a 2022 outbreak, first recorded in London, that affected 111 countries in Europe, South and North America, Africa, the Middle East, Asia and Oceania. More than 99% of people infected in that outbreak survived, because this clade of the virus is less deadly. Wealthy countries affected by the outbreak were also able to stockpile vaccines and antivirals for treatment.

Clade 1, however, is much more severe and could kill up to a tenth of those infected. This is the clade that typically appears in the DRC and is behind the current outbreak.
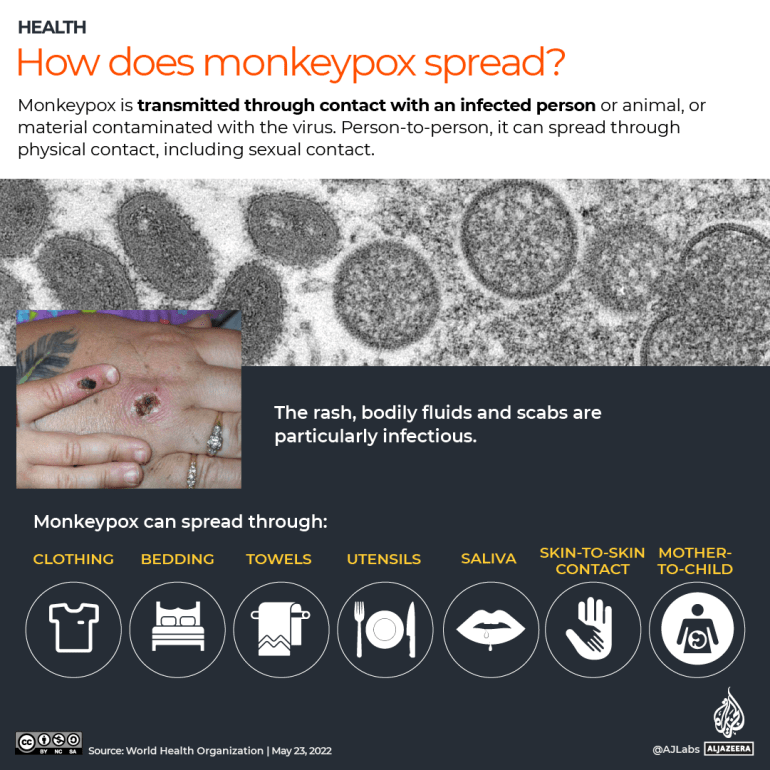
This variant of the virus is usually transmitted through normal physical contact. However, experts say infections are mainly spread through sexual contact in this outbreak.
This is especially true in the town of Kamituga, a hot spot with a large population of sex workers, said Dr. Jean Bisimwa Nachega, a professor of medicine at the University of Pittsburgh.
Kamituga is the same location where the new strain of Clade 1 classification was discovered in September 2023.
This is a “significant development,” Dr Nachega said, referring to the vulnerabilities of sex workers who, in addition to being economically disadvantaged and lacking access to health care, are also more likely than the rest of the population to have compromised immunity to diseases such as HIV.
“Unlike historical animal-to-human transmission, human-to-human sexual transmission, especially among high-risk groups such as sex workers, adds a new challenge to controlling the virus,” he said.
WHO says it is unclear whether this variant is more transmissible or causes more severe disease.
Doctors interviewed by The Associated Press said the new variant presents differently. Typically, MPOX lesions appear on the face, arms, chest and legs, and are clearly visible in an infected person. In this case, however, the lesions reported are largely on the genitals, experts said, making tracking and diagnosing cases much more difficult.
According to WHO, no cases of sexual transmission of clade I virus have been reported during previous outbreaks in the DRC. Cases reported in the country since the 1970s have mainly been due to ordinary direct contact with infected people or animals.
What are the main obstacles facing the authorities?
The eastern region of the DRC is also severely affected by conflict and has limited resources, making it difficult for authorities to adequately track, treat and monitor infected people, experts said. There are only two testing laboratories, in Kinshasa and Goma, and only 18% of reported cases have been tested in a laboratory.
WHO also said the country does not have enough treatment kits and vaccines. Tecovirimat, an antiviral drug licensed for smallpox, is currently being tested on more vulnerable patients in the DRC, according to WHO.
Vaccines can help minimize the spread and were key to containing the outbreak in 2022 that hit wealthier countries, such as the United Kingdom and the United States. But there are not enough vaccines to cover the DRC’s 100 million people. The country’s health minister has authorized doctors to administer available vaccines in areas most at risk. Officials said the DRC is in talks with countries, including Japan, to try to secure more vaccines.
Public awareness of MPOX is also limited, making self-reporting and isolation difficult. Some patients have left isolation to buy food or continue their work, experts said.
The fact that the disease can now be sexually transmitted adds an extra layer of stigma, a problem that dogged health workers during the initial spread of HIV/AIDS, experts said. They said there is a risk of “silent transmission” if people do not come forward themselves.

What are the risks for other African countries?
The eastern region of the DRC, which shares borders with Rwanda, Burundi, Uganda and Tanzania, is also a place of high mobility, with people moving in and out regularly, increasing the risk of transmission to other countries. To the south, the DRC borders Zambia and Angola, while its western and northern regions share borders with the Republic of Congo, the Central African Republic and South Sudan.
Like the DRC, many other African countries also have limited testing, treatment and surveillance capacities, making it an issue of regional and global concern, Dr Nachega said.
“Infectious diseases know no borders. Outbreaks in one region can quickly spread to other parts of the world, as seen with COVID-19. Although the current mpox outbreak appears to be contained in part of the DRC, populations across the continent must remain vigilant,” he added.
So far, 19 cases have been detected in neighboring Republic of Congo, which appears to have originated from the DRC, although this has not been confirmed. In April, authorities there declared a state of emergency.
In Cameroon, 23 cases of clade 2 virus were reported between January and April this year. South Africa also recorded five cases of clade 2 in an outbreak between January and May, although the WHO says there may be more undocumented cases.
These cases are likely not directly linked to the outbreak in the DRC. Travel between South Africa and the DRC for commercial purposes is common, but some experts believe these cases are linked to the 2022 global clade 2 outbreak.